Homeostenosis: A paradigm for understanding clinical vulnerability in aging adults in long-term care.
June 2023
Contributors: Dr. Henry Siu, with acknowledgements to Dr. Scott Nash
Summary:
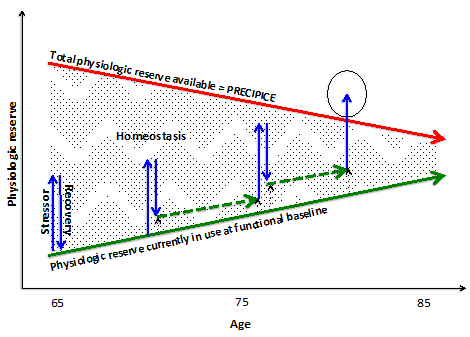
Homeostenosis was first described in the 1940s.1 Homeostenosis describes the narrowing (i.e., stenosis) of the older adult to maintain their function and physiologic baseline (i.e., homeostasis). It is a useful model for understanding and communicating why older adults become increasingly vulnerable to minor perturbations (physical, mental, social, other) with age. While this concept is not new in the world of Geriatric medicine, it is not often applied or discussed in field of long-term care (LTC) medicine. The concept of homeostenosis is demonstrated in the following diagram.
In the ideal world, every older adult would make a full recovery after a stressor. Unfortunately, this is not the case for older adults living in LTC homes. In this model, stressor (blue arrows) push an older adult towards the red arrow, which represents the amount of reserve available to deal with illness. When patients are younger, they often have a full recovery (i.e. returning back down to the solid green line). As patients get older, repeated stressors lessens their ability to fully recover. Each partial recovery results in a narrowing of the gap between the red and green arrows. Eventually, when a stressor pushes an older adult over the red arrow, clinically significant negative health outcomes occur. In LTC, homeostenosis provides a reason for why a resident can seem clinically well at one moment and then significantly ill the next.
For learners, homeostenosis demonstrates how physiologic aging, illnesses, geriatric syndromes (e.g. congestive heart failure, COPD, falls, multimorbidity, polypharmacy, delirium, etc), and the social determinants of health (e.g., poverty, education) can increase an older adult’s vulnerability by impacting the slopes of either the red and green arrows. Physiologic concepts associated with aging, such as sarcopenia, and the natural aging of all organ systems are inherently embedded in the red, downward sloping arrow. Chronic illnesses, like end-stage COPD or CHF, or multimorbidity would increase the slope of the green arrow (i.e. increase the baseline metabolic requirement). Furthermore, a learner can better appreciate the importance of learning about how evidence-based preventive measures could effectively increase the distance between the two arrows. Promoting immunizations, nutrition, and exercise guidelines2-5 becomes much more relevant to the clinician and learner when seen through this lens.
Familiarizing ourselves and our learners with the homeostenosis model will help us all be better communicators about clinical vulnerability to LTC residents and their families. Helping LTC residents and their families better understand clinical vulnerability would support efforts to avoid repeated and unnecessary hospital transfers and help dispel some prevalent myths around poor care provision in LTC homes. Helping LTC residents and their families acknowledge clinical vulnerability would align our care recommendations with a resident’s goals of care.
Take Away Tidbits:
This simple model can help learners understand clinical vulnerability in older adults in LTC. This model can be easily drawn on a sheet of paper when having serious-illness conversations with LTC residents and their families, making this a power and practical communication tool.
References:
1. Cowdry E. Problems of Ageing: Biological and Medical Aspects. 2nd ed. Baltimore: Williams & Wilkins; 1942.
2. Fulop T, Larbi A, Witkowski JM, McElhaney J, Loeb M, Mitnitski A, et al. Aging, frailty and age-related diseases. Biogerontology. 2010;11(5):547-63.
3. Bray NW, Smart RR, Jakobi JM, Jones GR. Exercise prescription to reverse frailty. Appl Physiol Nutr Metab. 2016;41(10):1112-6.
4. Dent E, Lien C, Lim WS, Wong WC, Wong CH, Ng TP, et al. The Asia-Pacific Clinical Practice Guidelines for the Management of Frailty. Journal of the American Medical Directors Association. 2017;18(7):564-75.
5. Konetzka RT, Spector W, Limcangco MR. Reducing hospitalizations from long-term care settings. Med Care Res Rev. 2008;65(1):40-66.